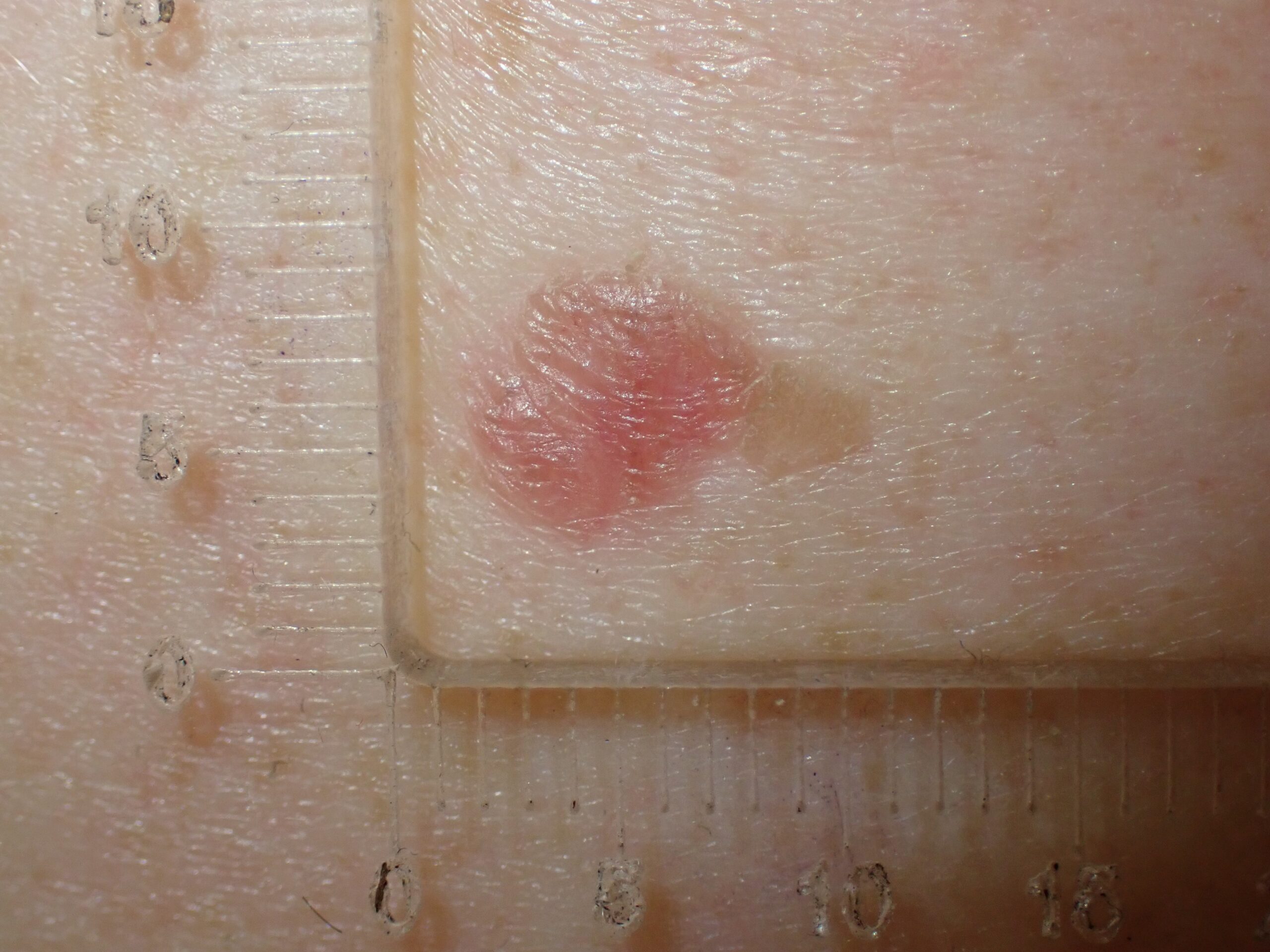
In this week’s case discussion from Dr David Stewart, we look at a 84-year-old male patient who was seen by another GP with a new tender lesion on the rim of his helix. That GP gave him antibiotics but the lesion didn’t improve.
The patient has a history of squamous cell carcinoma and lentigo maligna.
What do you think of this lesion? What would you do next?


Update
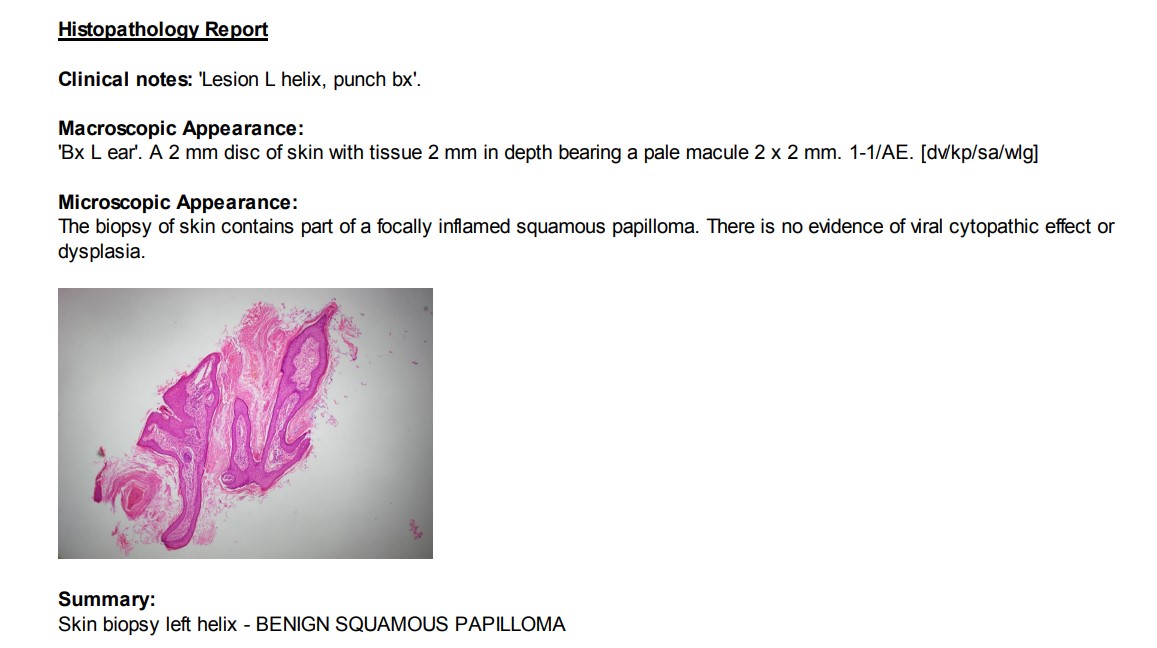
Here is the pathology result. As the management of benign lesions is important, too, what would you do next?
For further information on this topic, you may be interested to learn more about the HealthCert Professional Diploma program in Skin Cancer Medicine.
 Would you like to obtain advice or share your experience with your colleagues in the weekly blog case discussion, moderated by Dr Terry Harvey?
Would you like to obtain advice or share your experience with your colleagues in the weekly blog case discussion, moderated by Dr Terry Harvey?
Participate with your cases so that we can learn together!
Submit your case here or send details to admin@healthcert.com


 1800 867 1390
1800 867 1390

 Would you like to obtain advice or share your experience with your colleagues in the weekly blog case discussion, moderated by Dr Terry Harvey?
Would you like to obtain advice or share your experience with your colleagues in the weekly blog case discussion, moderated by Dr Terry Harvey?