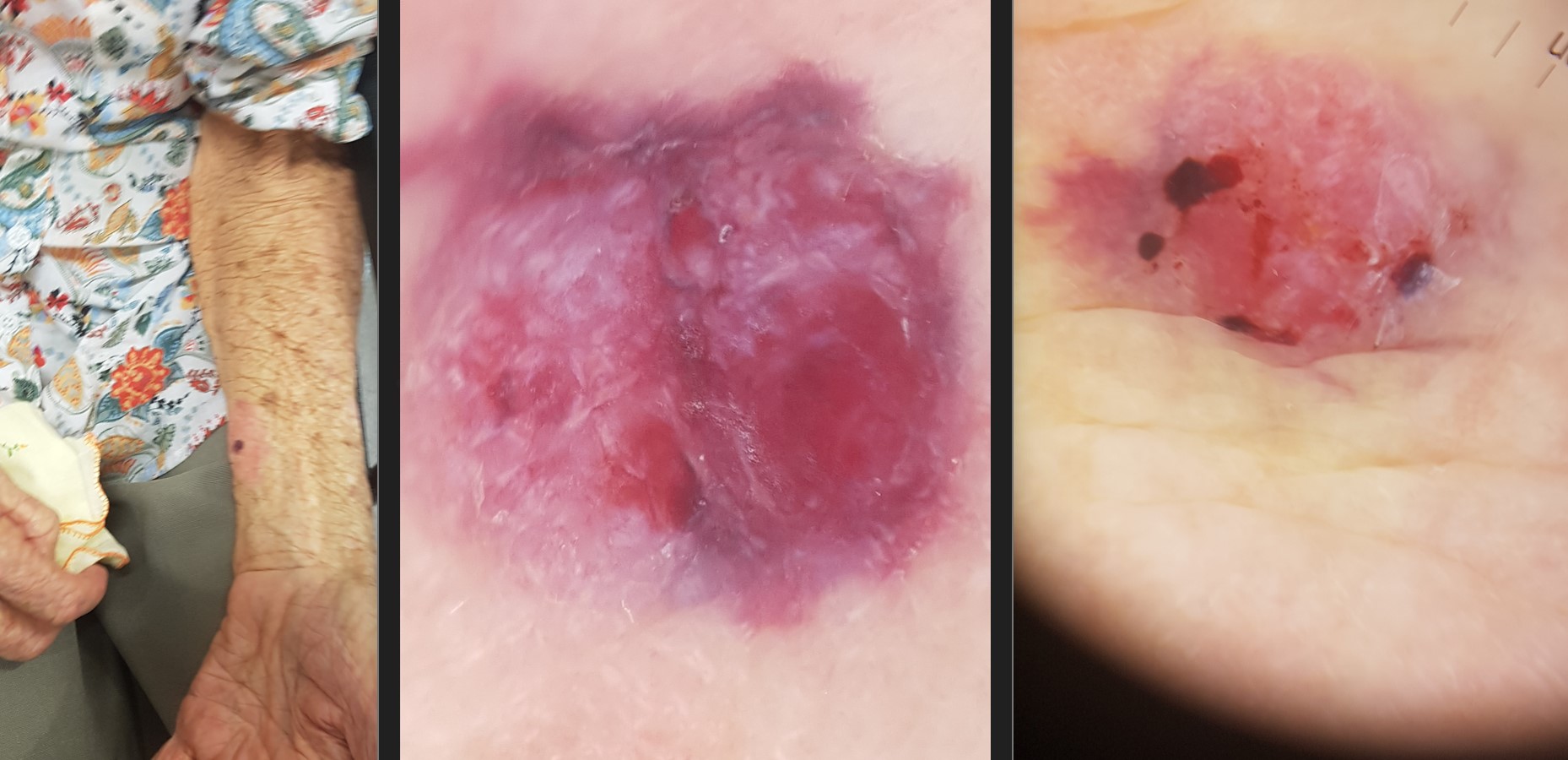
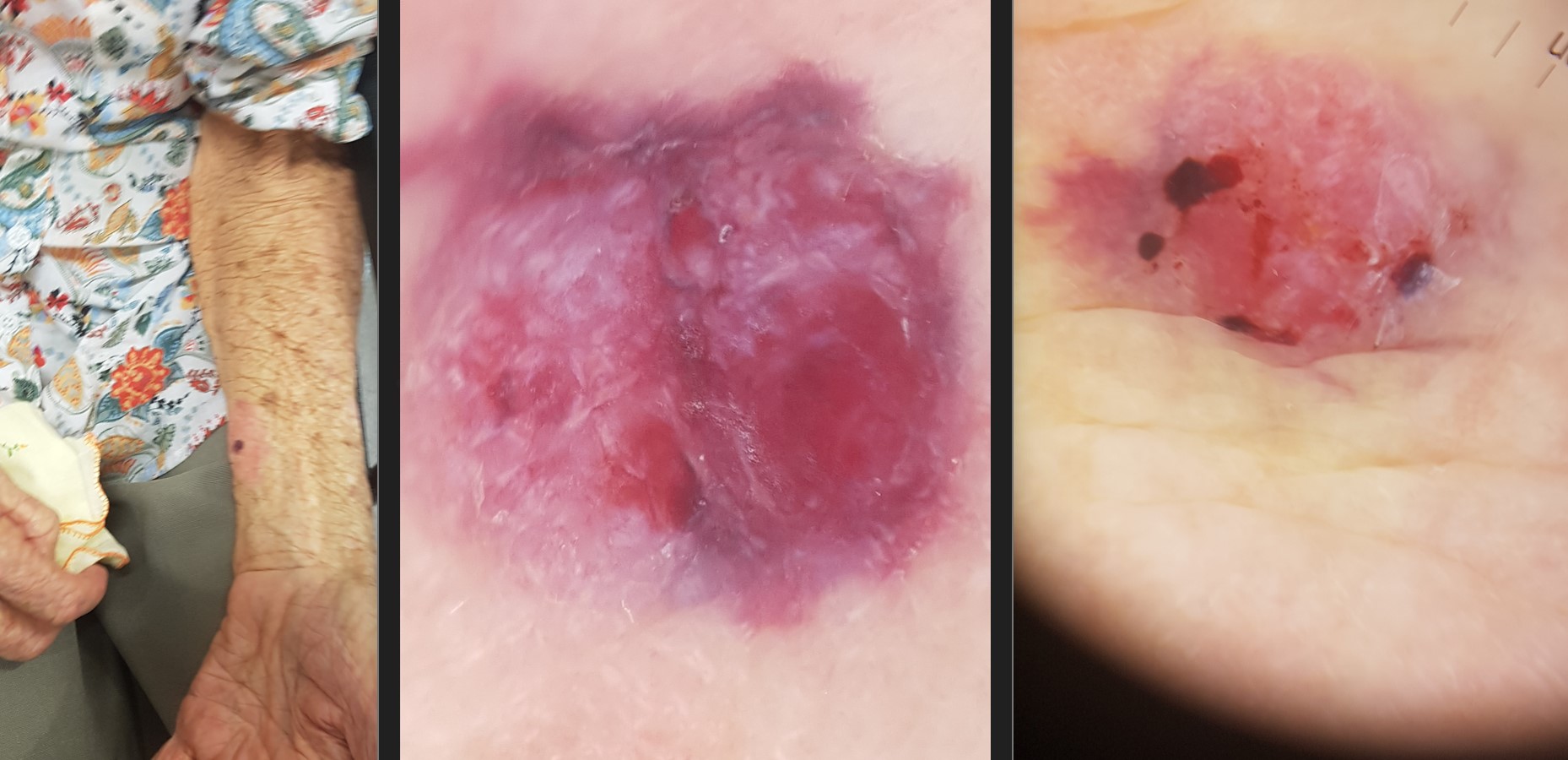
In this week's discussion, submitted by Dr Renuka Ranasinghe, we look at the challenging case of an 88-year-old lady with Dementia and Parkinson's Disease who came in for a skin check. She is wheelchair bound, and frequent writhing movements were an issue during examination and treatment (therefore, apologies for the blur in the photos).
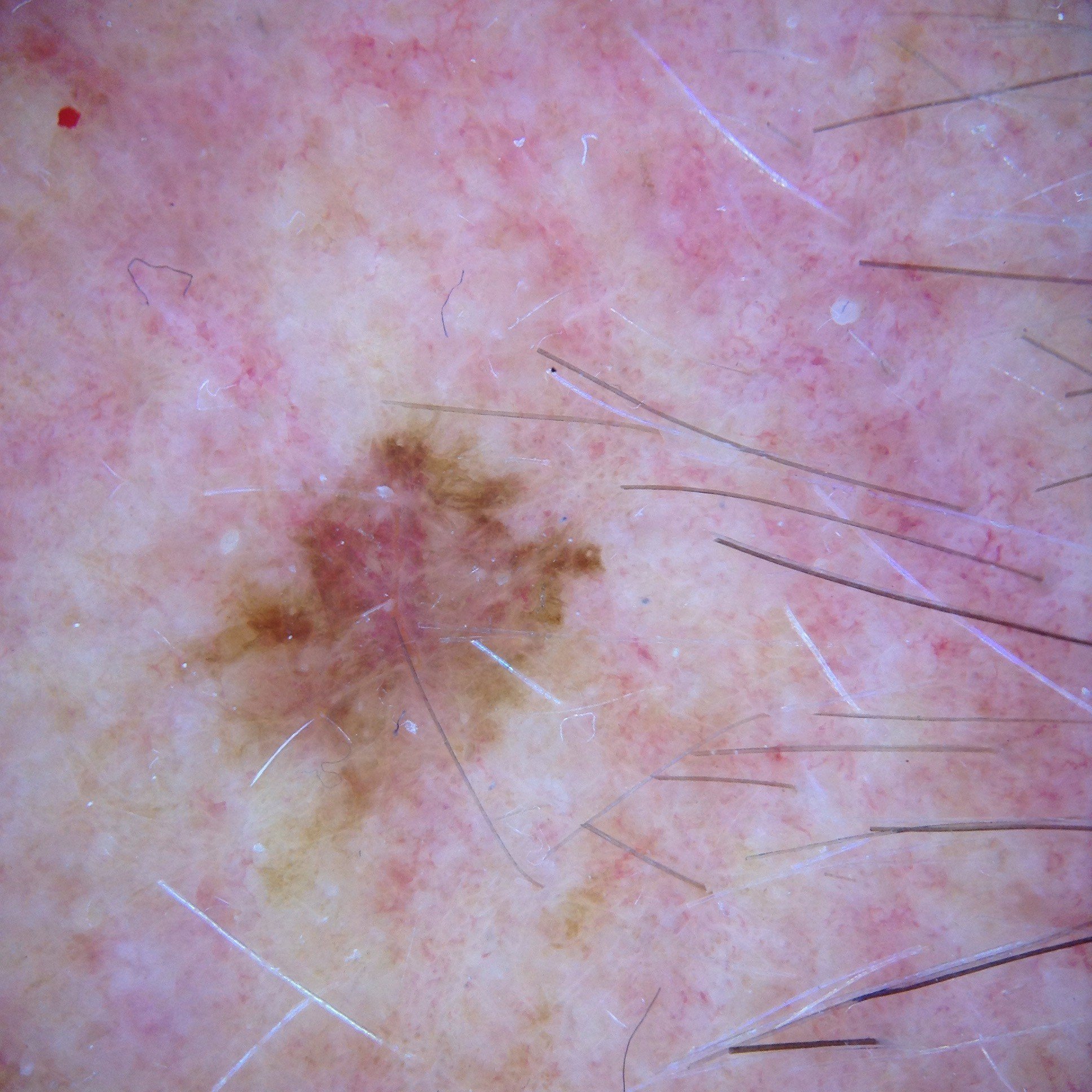
According to the patient's daughter, a pink nodular lesion on the patient's arm had remained unchanged for years but had shown noticeable change over the past few weeks. The photos below show the dermoscopic change that occurred between the patient's initial skin exam and a follow-up check two weeks later.
What are your thoughts here? With consideration of the patient's other conditions, how would you manage this case?
Update:
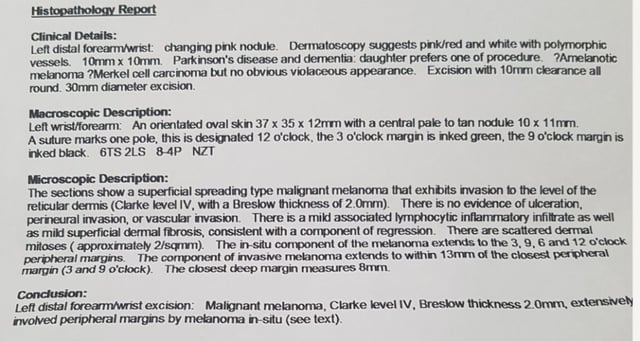
Here is the pathology report:
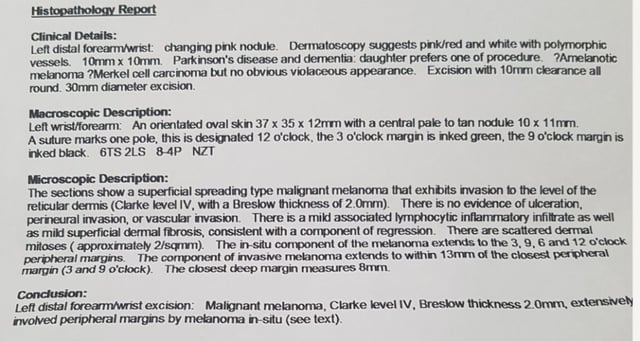
The patient's family wanted one-off surgery due to her clinical condition.
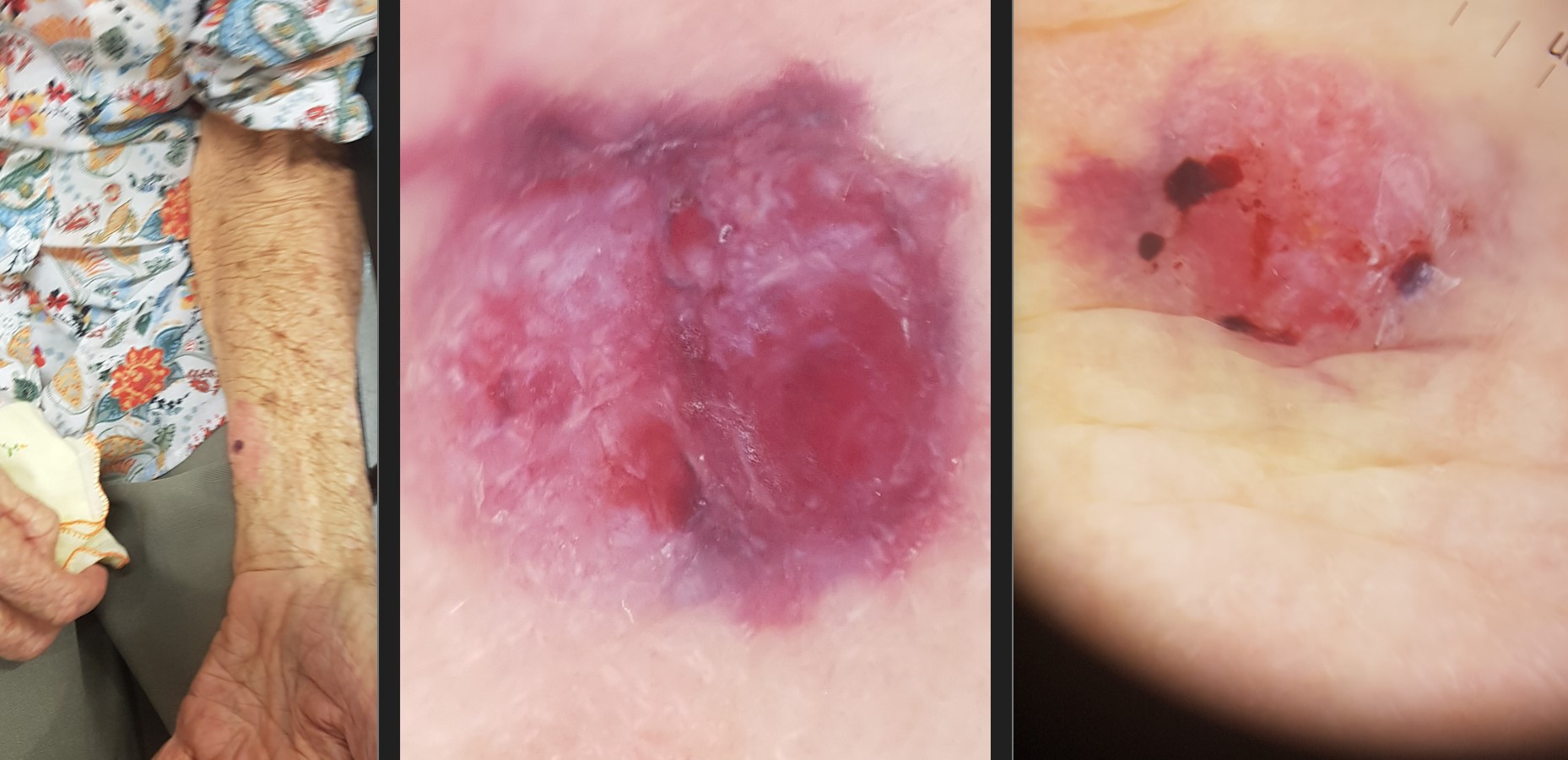
The invasive melanoma was fully excised with 13mm closest peripheral margin and 8mm deep margin clearance. Closed with rhomboid flap from volar aspect of forearm.
Melanoma in situ extends to the peripheral margins. Referred to MDT team in Perth and awaiting advice.
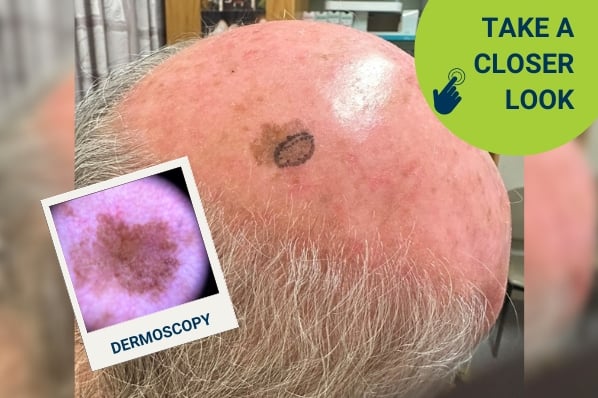
Post-surgery photos:


For further information on this topic, you may be interested to learn more about the HealthCert Professional Diploma program in Skin Cancer Medicine.

Would you like to obtain advice or share your experience with your colleagues in the weekly blog case discussion?
Participate with your cases so that we can learn together!
Submit your case here or send details to admin@healthcert.com

 1800 867 1390
1800 867 1390